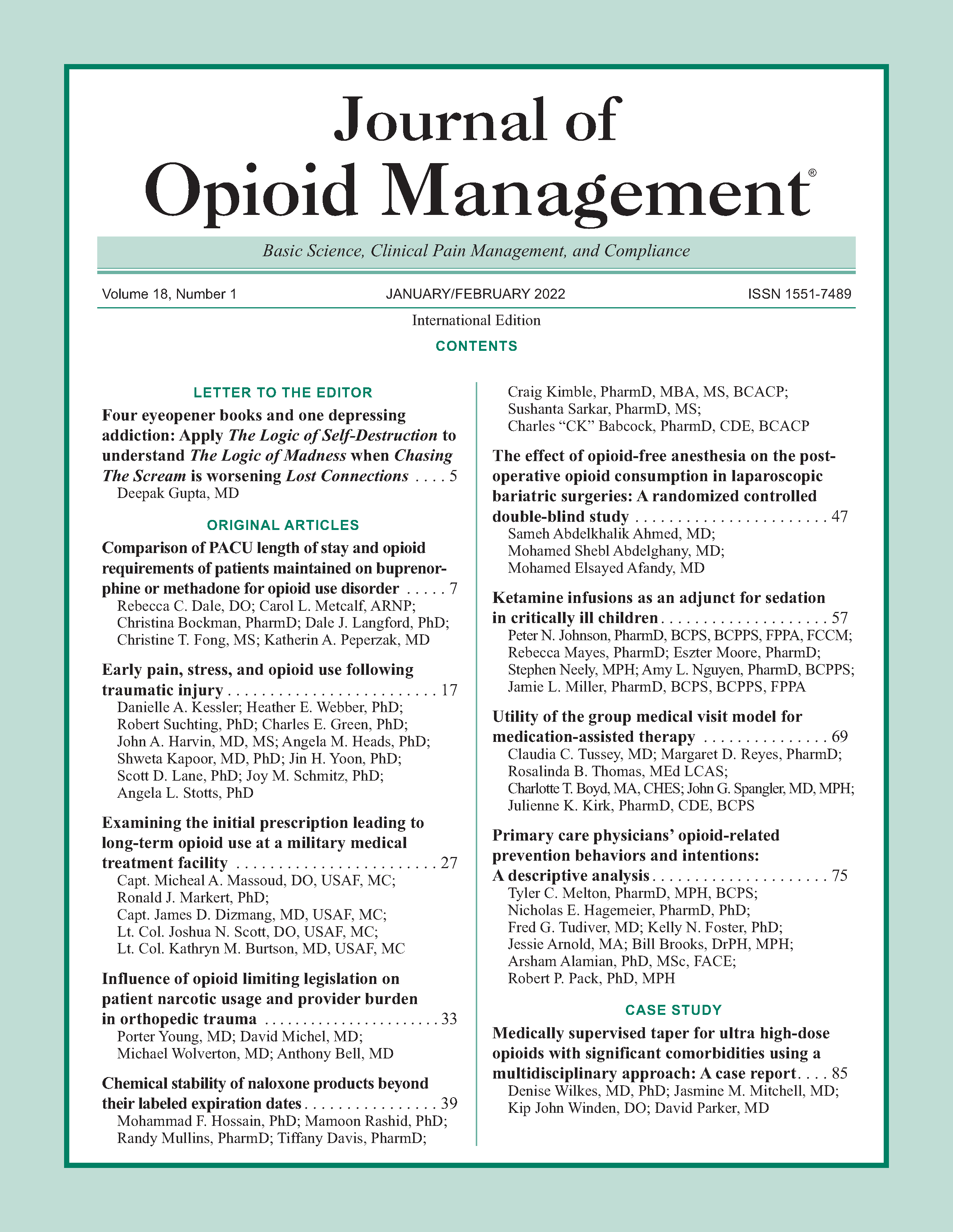
Primary care physicians’ opioid-related prevention behaviors and intentions: A descriptive analysis
DOI:
https://doi.org/10.5055/jom.2022.0697Keywords:
primary care physicians, opioid use disorder, primary prevention, secondary prevention, tertiary preventionAbstract
Objective: Primary care physicians (PCPs) are positioned to mitigate opioid morbidity and mortality, but their engagement in primary, secondary, and tertiary opioid-related prevention behaviors is unclear. The objective of this study was to evaluate Tennessee PCPs’ engagement in and intention to engage in multiple opioid-related prevention behaviors.
Methods: A survey instrument was developed, pretested, and pilot tested with practicing PCPs. Thereafter, a census of eligible Tennessee PCPs was conducted using a modified, four-wave tailored design method approach. Three patient scenarios were employed to assess physician intention to engage in 10 primary, secondary, and tertiary prevention behaviors. Respondents were asked to report, given 10 similar scenarios, the number of times (0-10) they would engage in prevention behaviors. Descriptive statistics were calculated using SPSS version 25.
Results: A total of 296 usable responses were received. Physician intention to engage in prevention behaviors varied across the 10 behaviors studied. Physicians reported frequently communicating risks associated with prescription opioids to patients (8.9 ± 2.8 out of 10 patients), infrequently utilizing brief questionnaires to assess for risk of opioid misuse (1.7 ± 3.3 out of 10 patients), and screening for current opioid misuse (3.1 ± 4.3 out of 10 patients). Physicians reported seldomly co-prescribing naloxone for overdose reversal and frequently discharging from practice patients presenting with an opioid use disorder.
Conclusions: This study noted strengths and opportunities to increase engagement in prevention behaviors. Understanding PCPs’ engagement in opioid-related prevention behaviors is important to effectively target and implement morbidity and mortality reducing interventions.
References
Rudd RA, Aleshire N, Zibbell JE, et al.: Increases in drug and opioid overdose deaths–United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016; 64(50-51): 1378-1382. DOI: 10.15585/mmwr.mm6450a3.
Rudd RA, Seth P, David F, et al.: Increases in drug and opioid-involved overdose deaths—United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016; 65(50-51): 1445-1452. DOI: 10.15585/mmwr.mm655051e1.
Paulozzi LC, Jones C, Mack K, et al.: Signs: Overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011; 60(43): 1487-1492.
Theisen K, Jacobs B, Macleod L, et al.: The United States opioid epidemic: A review of the surgeon's contribution to it and health policy initiatives. BJU Int. 2018; 122(5): 754-759. DOI: 10.1111/bju.14446.
Scholl L, Seth P, Kariisa M, et al.: Drug and opioid-involved overdose deaths—United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018; 67(5152): 1419-1427. DOI: 10.15585/mmwr.mm675152e1.
Murphy S, Xu J, Kochanek K, et al.: Mortality in the United States, 2017. NCHS Data Brief. 2018; 328: 1-8.
Califf RM, Woodcock J, Ostroff S: A proactive response to prescription opioid abuse. N Engl J Med. 2016; 374(15): 1480-1485. DOI: 10.1056/NEJMsr1601307.
Centers for Disease Control and Prevention: CDC Prevention- Picture of America. https://www.cdc.gov/pictureofamerica/pdfs/picture_of_america_prevention.pdf. Updated April 6, 2017. Accessed May 13, 2019.
Saloner B, McGinty EE, Beletsky L, et al.: A public health strategy for the opioid crisis. Public Health Rep. 2018; 133(1_suppl): 24s-34s. DOI: 10.1177/0033354918793627.
Hurstak EE, Kushel M, Chang J, et al.: The risks of opioid treatment: Perspectives of primary care practitioners and patients from safety-net clinics. Subst Abuse. 2017; 38(2): 213-221. DOI: 10.1080/08897077.2017.1296524.
Cheatle MD, Barker C: Improving opioid prescription practices and reducing patient risk in the primary care setting. J Pain Res. 2014; 7: 301-311. DOI: 10.2147/jpr.s37306.
Dowell D, Zhang K, Noonan RK, et al.: Mandatory provider review and pain clinic laws reduce the amounts of opioids prescribed and overdose death rates. Health Aff (Millwood). 2016; 35(10): 1876-1883. DOI: 10.1377/hlthaff.2016.0448.
Kolodny A, Courtwright DT, Hwang CS, et al.: The prescription opioid and heroin crisis: A public health approach to an epidemic of addiction. Annu Rev Public Health. 2015; 36: 559-574. DOI: 10.1146/annurev-publhealth-031914-122957.
Gordis L: Epidemiology. 5th ed. Philadelphia, PA: Elsevier/Saunders, 2014.
Dillman DA, Smyth JD, Christian LM: Internet, Phone, Mail, and Mixed Mode Surveys: The Tailored Design Method. 4th ed. Hoboken, NJ: John Wiley & Sons Inc, 2014.
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association, 2013.
The American Association for Public Opinion Research: Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 9th ed. Oakbrook Terrace: AAPOR, 2016.
Hero JO, McMurtry C, Benson J, et al.: Discussing opioid risks with patients to reduce misuse and abuse: Evidence from 2 surveys. Ann Fam Med. 2016; 14(6): 575-577. DOI: 10.1370/afm.1994.
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic Pain - United States, 2016. MMWR Recomm Rep. 2016; 65(1): 1-49. DOI: 10.15585/mmwr.rr6501e1.
McCalmont JC, Jones KD, Bennett RM, et al.: Does familiarity with CDC guidelines, continuing education, and provider characteristics influence adherence to chronic pain management practices and opioid prescribing? J Opioid Manag. 2018; 14(2): 103-116. DOI: 10.5055/jom.2018.0437.
Miller NS, Sheppard LM, Colenda CC, et al.: Why physicians are unprepared to treat patients who have alcohol- and drug-related disorders. Acad Med. 2001; 76(5): 410-418. DOI: 10.1097/00001888-200105000-00007.
Wakeman SE, Pham-Kanter G, Donelan K: Attitudes, practices, and preparedness to care for patients with substance use disorder: Results from a survey of general internists. Subst Abuse. 2016; 37(4): 635-641. DOI: 10.1080/08897077.2016.1187240.
McNeely J, Kumar PC, Rieckmann T, et al.: Barriers and facilitators affecting the implementation of substance use screening in primary care clinics: A qualitative study of patients, providers, and staff. Addict Sci Clin Pract. 2018; 13(1): 8. DOI: 10.1186/s13722-018-0110-8.
Thiesset HF, Schliep KC, Stokes SM, et al.: Opioid misuse and dependence screening practices prior to surgery. J Surg Res. 2020; 252: 200-205. DOI: 10.1016/j.jss.2020.03.015.
Klimas J, Gorfinkel L, Fairbairn N, et al.: Strategies to identify patient risks of prescription opioid addiction when initiating opioids for pain: A systematic review. JAMA Netw Open. 2019; 2(5):e193365. DOI: 10.1001/jamanetworkopen.2019.3365.
Arnold RM, Han PK, Seltzer D: Opioid contracts in chronic nonmalignant pain management: Objectives and uncertainties. Am J Med. 2006; 119(4): 292-296. DOI: 10.1016/j.amjmed.2005.09.019.
Wicclair M: Dismissing patients for health-based reasons. Camb Q Healthc Ethics. 2013; 22(3): 308-318. DOI: 10.1017/s0963180113000121.
Lagisetty PA, Healy N, Garpestad C, et al.: Access to primary care clinics for patients with chronic pain receiving opioids. JAMA Netw Open. 2019; 2(7):e196928. DOI: 10.1001/jamanetworkopen.2019.6928.
Jamison RN, Scanlan E, Matthews ML, et al.: Attitudes of primary care practitioners in managing chronic pain patients prescribed opioids for pain: A prospective longitudinal controlled trial. Pain Med. 2015; 17(1): 99-113. DOI: 10.1111/pme.12871.
Darnall BD, Juurlink D, Kerns RD, et al.: International stakeholder community of pain experts and leaders call for an urgent action on forced opioid tapering. Pain Med. 2019; 20(3): 429-433. DOI: 10.1093/pm/pny228.
Binswanger IA, Glanz JM, Faul M, et al.: The association between opioid discontinuation and heroin use: A nested case-control study. Drug Alcohol Depend. 2020; 217: 108248. DOI: 10.1016/j.drugalcdep.2020.108248.
Blevins CE, Rawat N, Stein MD: Gaps in the substance use disorder treatment referral process: Provider perceptions. J Addict Med. 2018; 12(4): 273-277. DOI: 10.1097/adm.0000000000000400.
Tennant F: When to Call in the Cavalry-When and Why to Refer a Patient for Pain Care. Montclair: Practical Pain Management, 2019.
Guy GP Jr, Haegerich TM, Evans ME, et al.: Vital signs: Pharmacy-based naloxone dispensing—United States, 2012-2018. MMWR Morb Mortal Wkly Rep. 2019; 68(31): 679-686. DOI: 10.15585/mmwr.mm6831e1.
Behar E, Bagnulo R, Coffin PO: Acceptability and feasibility of naloxone prescribing in primary care settings: A systematic review. Prev Med. 2018; 114: 79-87. DOI: 10.1016/j.ypmed.2018.06.005.
Groves RM: Nonresponse rates and nonresponse bias in household surveys. Public Opin Q. 2006; 70(5): 646-675. DOI: 10.1093/poq/nfl033.
Starrels JL, Becker WC, Weiner MG, et al.: Low use of opioid risk reduction strategies in primary care even for high risk patients with chronic pain. J Gen Intern Med. 2011; 26(9): 958-964. DOI: 10.1007/s11606-011-1648-2.
Published
How to Cite
Issue
Section
License
Copyright 2005-2024, Weston Medical Publishing, LLC
All Rights Reserved