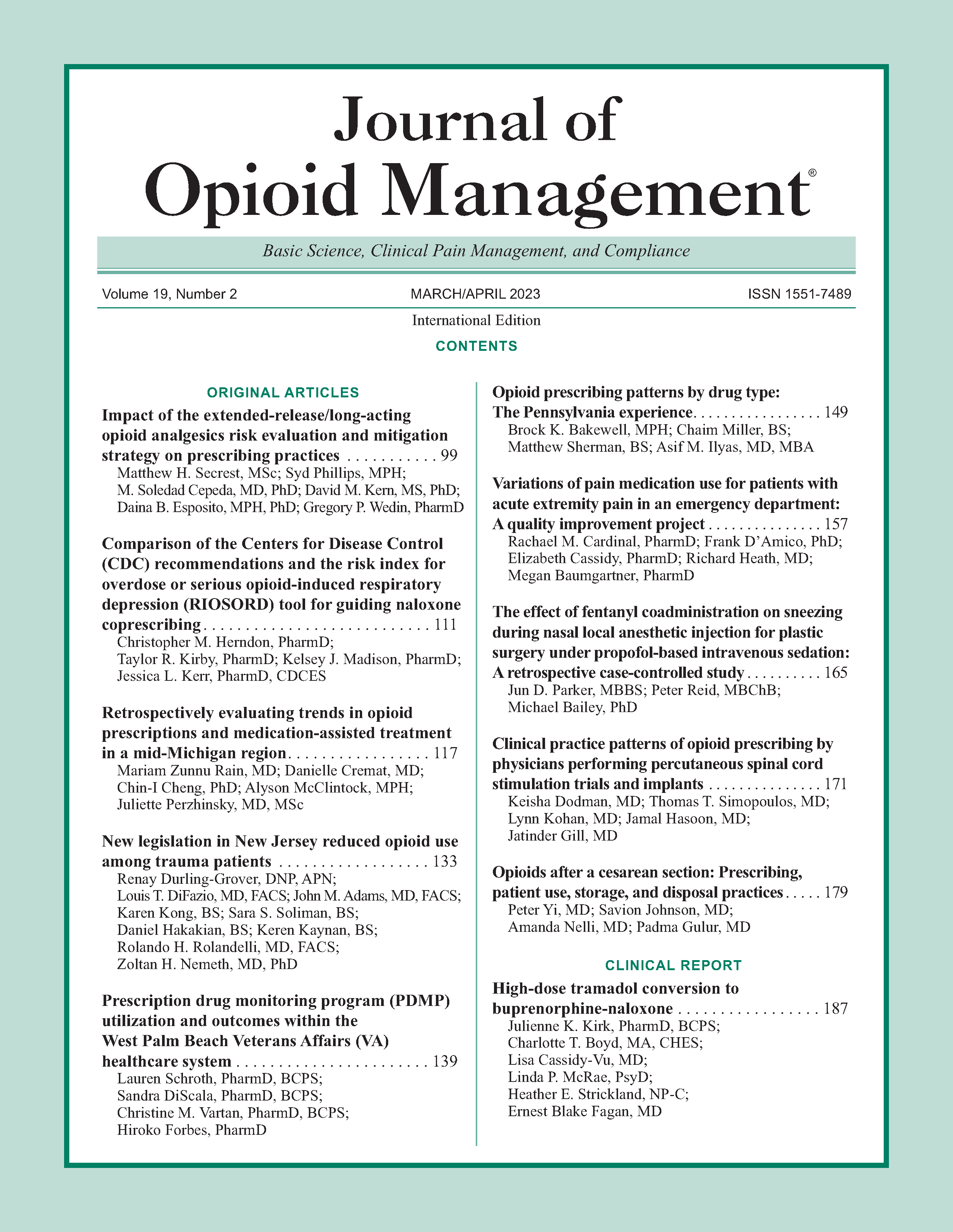
Opioid prescribing patterns by drug type: The Pennsylvania experience
DOI:
https://doi.org/10.5055/jom.2023.0769Keywords:
opioids, narcotics, prescribing, prescriptions, PDMP, PennsylvaniaAbstract
Objective: To explore the impact on opioid prescribing patterns and trends after implementing a prescription drug monitoring program (PDMP) in Pennsylvania from 2016 to 2020.
Design: A cross-sectional data analysis using deidentified data from Pennsylvania’s PDMP delivered by the Pennsylvania Department of Health was undertaken.
Setting: Data were collected from the entire state of Pennsylvania, and statistics were run at Rothman Orthopedic Institute Foundation for Opioid Research & Education.
Interventions: Evaluating the effect on opioid prescriptions after introduction of the PDMP.
Main outcome measure: In 2016, nearly 2 million opioid prescriptions were given to patients across the state. However, by the end of the study period in 2020, there was a 38 percent decrease in opioid prescriptions written.
Results: Beginning with Q3 2016, each subsequent quarter saw fewer opioids prescribed, decreasing on average by 3.4 ± 1.7 percent through Q1 2020. Specifically, over 700,000 fewer prescriptions were in the first quarter of 2020 compared to the third quarter in 2016. The opioids that were most frequently prescribed were oxycodone, hydrocodone, and morphine.
Conclusion: While fewer prescriptions were being prescribed overall, the breakdown of drug type being prescribed remained similar in 2020 compared to 2016. Fentanyl and hydrocodone saw the largest decrease between 2016 and 2020.
References
Centers for Disease Control: Wide-ranging online data for epidemiologic research (WONDER). 2020. Available at http://wonder.cdc.gov. Accessed December 3, 2020.
Hedegaard H, Miniño A, Warner M: Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief. 2020. Available at https://www.cdc.gov/nchs/data/databriefs/db356-h.pdf. Accessed January 19, 2021.
Wilson N, Kariisa M, Seth P, et al.: Drug and opioid-involved overdose deaths—United States, 2017-2018. MMWR Morb Mortal Wkly Rep. 2020; 69(11): 290-297. DOI: 10.15585/mmwr.mm6911a4.
Guy GP, Zhang K, Bohm MK, et al.: Vital signs: Changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017; 66(26): 697-704. DOI: 10.15585/mmwr.mm6626a4.
Preuss CV, Kalava A, King KC: Prescription of controlled substances: Benefits and risks. In StatPearls. Treasure Island, FL: StatPearls Publishing LLC, 2020.
Centers for Disease Control and Prevention: 2018 annual surveillance report of DrugpRelated risks and outcomes. 2018. Available at https://www.cdc.gov/drugoverdose/pdf/pubs/2018-cdc-drug-surveillance-report.pdf. Accessed January 20, 2021.
Reisman RM, Shenoy PJ, Atherly AJ, et al.: Prescription opioid usage and abuse relationships: An evaluation of state prescription drug monitoring program efficacy. Subst Abuse. 2009; 3: 41-51.
Surratt HL, O’Grady C, Kurtz SP, et al.: Reductions in prescription opioid diversion following recent legislative interventions in Florida. Pharmacoepidemiol Drug Saf. 2014; 23(3): 314-320. DOI: 10.1002/pds.3553.
Reifler LM, Droz D, Bailey JE, et al.: Do prescription monitoring programs impact state trends in opioid abuse/misuse? Pain Med. 2012; 13(3): 434-442. DOI: 10.1111/j.1526-4637.2012.01327.x.
National Institute on Drug Abuse: Prescription opioids DrugFacts: National Institute on Drug Abuse Website Web Site. 2020. Available at https://www.drugabuse.gov/publications/drugfacts/prescription-opioids. Accessed February 8, 2021.
Centers for Disease Control and Prevention: US opioid dispensing rate maps. 2020. Available at https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html#:~:text=Thepercent20overallpercent20nationalpercent20opioidpercent20dispensingpercent20ratepercent20declinedpercent20frompercent202012percent20to,thanpercent20153percent20millionpercent20opioidpercent20prescriptions). Accessed January 20, 2021.
Champagne-Langabeer T, Madu R, Giri S, et al.: Opioid prescribing patterns and overdose deaths in Texas. Substance Abuse. 2021; 42: 161-167. DOI: 10.1080/08897077.2019.167.5114.
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016; 315(15): 1624-1645. DOI: 10.1001/jama.2016.1464.
Finley EP, Garcia A, Rosen K, et al.: Evaluating the impact of prescription drug monitoring program implementation: A scoping review. BMC Health Serv Res. 2017; 17(1): 420. DOI: 10.1186/s12913-017-2354-5.
Delcher C, Wagenaar AC, Goldberger BA, et al.: Abrupt decline in oxycodone-caused mortality after implementation of Florida’s prescription drug monitoring program. Drug Alcohol Dependence. 2015; 150: 63-68. DOI: 10.1016/j.drugalcdep.2015.02.010.
Rasubala L, Pernapati L, Velasquez X, et al.: Impact of a mandatory prescription drug monitoring program on prescription of opioid analgesics by dentists. PLoS One. 2015; 10(8): e0135957. DOI: 10.1371/journal.pone.0135957.
Ringwalt C, Schiro S, Shanahan M, et al.: The use of a prescription drug monitoring program to develop algorithms to identify providers with unusual prescribing practices for controlled substances. J Primary Prevent. 2015; 36(5): 287-299. DOI: 10.1007/s10935-015-0397-0.
Stein BD, Taylor EA, Sheng F, et al.: Change in per capita opioid prescriptions filled at retail pharmacies, 2008-2009 to 2017-2018. Ann Intern Med. 2022; 175(2): 299-302. DOI: 10.7326/M21-3042.
Langabeer J, Gourishankar A, Chambers K, et al.: Disparities between US opioid overdose deaths and treatment capacity: A geospatial and descriptive analysis. J Addict Med. 2019; 13(6): 476-482. DOI: 10.1097/ADM.0000000000000523.
Feldman L, Williams KS, Coates J, et al.: Awareness and utilization of a prescription monitoring program among physicians. J Pain Palliative Care Pharmacother. 2011; 25(4): 313-317. DOI: 10.3109/15360288.2011.606292.
Lagisetty PA, Healy N, Garpestad C, et al.: Access to primary care clinics for patients with chronic pain receiving opioids. JAMA Netw Open. 2019; 2(7): e196928. DOI: 10.1001/jamanetworkopen.2019.6928.
Freeman J: Drug diverting patients & prescription monitoring—Both sides of the debate. Iowa Med J Iowa Med Soc. 2004; 94(5): 10-11.
Perrone J, Nelson LS: Medication reconciliation for controlled substances—An “ideal” prescription-drug monitoring program. N Engl J Med. 2012; 366(25): 2341-2343. DOI: 10.1056/NEJMp1204493.
Dasgupta N, Creppage K, Austin A, et al.: Observed transition from opioid analgesic deaths toward heroin. Drug Alcohol Depend. 2014; 145: 238-241. DOI: 10.1016/j.drugalcdep.2014.10.005.
Oquendo MA, Volkow ND: Suicide: A silent contributor to opioid-overdose deaths. N Engl J Med. 2018; 378(17): 1567-1569. DOI: 10.1056/NEJMp1801417.
Published
How to Cite
Issue
Section
License
Copyright 2005-2024, Weston Medical Publishing, LLC
All Rights Reserved